The US Federal government departments released mandates for Health Plans or Issuers to provide better consumer coverage transparency. Plans must disclose cost-sharing information to enrollees, beneficiaries, or participants related to the covered services. Issuers also need to publish in-network negotiated rates, historical out-of-network allowed amounts, and prescription drug pricing based on each provider's contracts and plans offered. The disclosed information is essential for hospital regulatory compliance, guiding consumers to make better decisions regarding services, providers, and their health. Health Plans need to integrate their internal systems to achieve compliance.
Milestones on the Timeline
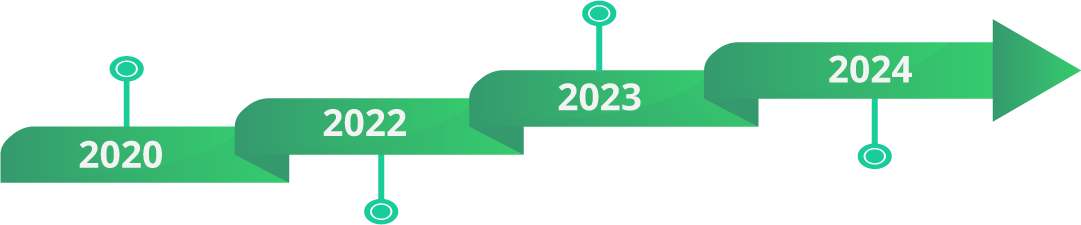
MLR Calculation Update
Effective with the 2020 MLR reporting year
Disclosure to Public
Applicable for Plan years beginning on or after
Jan 1, 2022
Disclosure to Enrollees
Jan 1, 2023 – Applicable to 500 Pre-defined items or services
Disclosure to Enrollees
Jan 1, 2024 – Applicable to
all items or services
Key Elements of Transparency in Coverage for Hospitals

Machine Readable Files
Hospitals must regularly publish machine-readable files with standard charges, including gross, discounted, and negotiated prices.

Shoppable Services
Hospitals must offer pricing estimates for at least 300 pre-defined services, allowing patients to compare costs across providers.

Compliance Penalties
Hospitals face civil penalties for non-compliance. Timely updates and addressing gaps in pricing information are essential.

Good Faith Estimates
Hospitals must provide comprehensive cost estimates for uninsured or self-paying patients under the No Surprises Act.

Consumer Tools
Online cost estimator tools should be user-friendly and reflect current out-of-pocket costs for patients.
Requirements
How Can You Achieve It?
To ensure that your solution fulfills future requirements, below are the vital elements you need to account for in your technology roadmap.
Enterprise Applications Integration
Authentication and Authorization
Content & Vocabulary Mappings
Data
Management
Error Handling
Audit
FHIR
We Can Help With Compliane Plans for Healthcare Organizations
Assessment
Compliance gap identification, and process blueprinting
Roadmap Planning
Chart out an execution plan with milestones
Implementation
Leverage technology to realize the roadmap
Go-Live and Support
Performance consistency and continuous improvement
Let’s Talk
Ensure your systems and processes are healthcare insurance compliant!
Connect with us and let us make this endeavor a cakewalk for you!
Worth Exploring
A glimpse of our industry expertise
