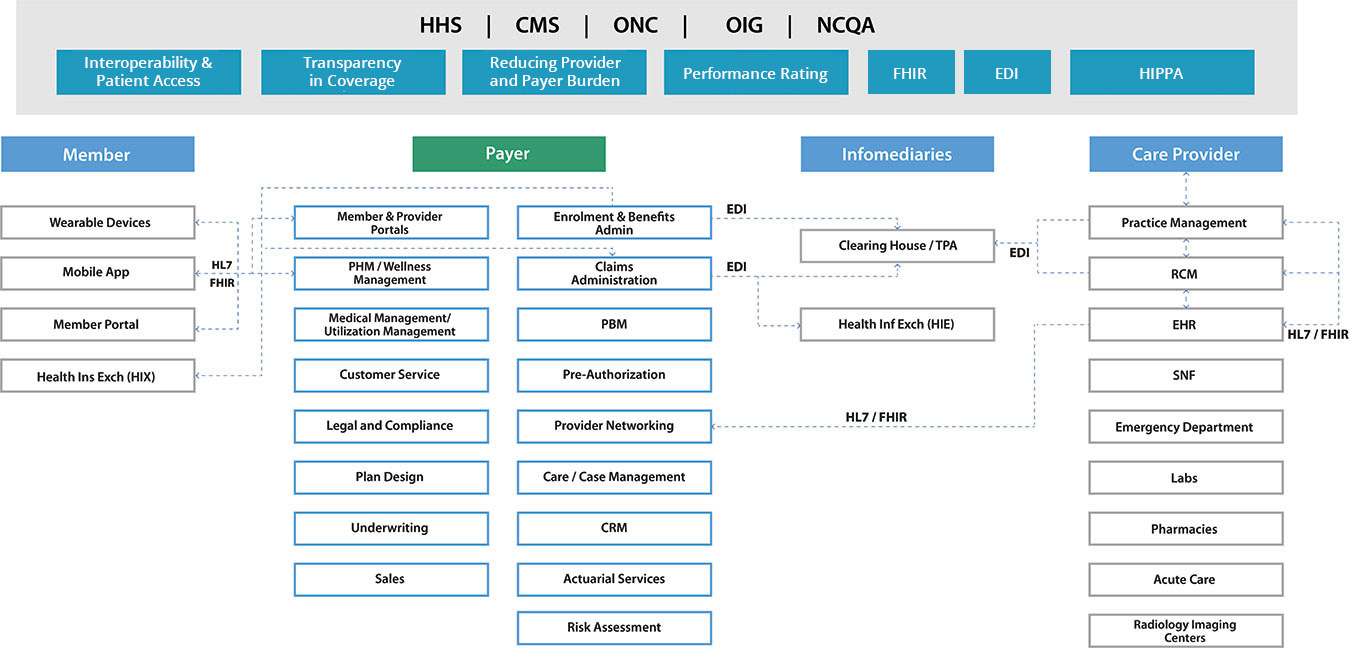
Healthcare payer solutions are applications and systems that enable healthcare insurance companies or payers to manage various aspects of their business, such as claims processing, member management, provider networks, and payment processing. These solutions help payers optimize their operations, improve member satisfaction, and reduce costs.
The US healthcare payer environment has been subjected to waves of changes. We help payers traverse these changes by connecting people, processes, and technology to power exceptional member experience with greater efficiency. Innovation in ideas, agility in execution, quality of deliverables and judicious use of resources are implicit centrepieces for success. These are the ingredients we bring to all our relationships at Nalashaa. The Covid-19 pandemic has forced payers to rethink their IT strategies and be flexible for any unseen future events.
Payer Solutions to Accelerate Your Business
- Integrate various sources for Clinical, Financial, Administrative, Member, Provider and operations data using standards such as FHIR, HL7, EDI
- Aggregation, segregation, classification and management of data with BI, AI/ML, etc.
- Deductive and predictive analysis of data for scientific decision-making
- Meaningful presentation to enable quick business decisions using dashboards and self-service reporting
- Support existing applications (even legacy ones - AS400, Delphi, VB etc.)
- Document and reverse-engineer legacy solutions
- Build wrapper applications to provide a modern user experience while maintaining the robust, time-tested back-end
- Provide SLA-bound sunset support

- Architect, Design and Develop solutions using modern technologies
- Technology migration of solutions
- Migrate/Extend existing applications to cloud/mobile
- Perform independent validation and verification of developed solutions
- Uplift/Enhance User Experience of existing solutions

- Identify, Stratify, Classify and Positively Impact the health of high-risk members through well designed population health management solutions
- Successfully use and report Health Plan Performance measures
- Manage your provider networks and contracts to maximize quality ratings and your bottom-line
- Benchmark performance and identify instances of fraud, gaps in processes, which results in sour provider relationships
- Increase consumer health awareness by integrating better with provider system
- Ensure consumer participation in your outreach programs through professional CRM initiatives
- Enhance your reach through mobile solutions and gain more consumer eyeballs to drive preventive measures
- Listen better to your members by tracking their actions through ‘Internet of Things’ (IoT) enabled devices

Why choose Nalashaa
From experience, we have noticed that often HIT organizations miss out on a few things that should be implicit expectations from healthcare software development companies as their partner
400+
Healthcare Software Developed
13Yrs+
Experience in Healthcare
15M+
Unique patients touched
25K+
Clinics using our Solution
8M+
Man-hours in software development
Compliance Experience
HIPAA, GDPR, NCPDP, FDA, ONC, MDR, SAMHSA, IVDR, MACRA, MIPS, CEHRT, SAFER and HTI-1.
Standards Proficiency
HL7, ICD-10, LOINC, CPT, XDS/XDS-I, FHIR, DICOM, Blue Button+, CDA, and CCD.
ISO certifications
ISO 9001:2015
ISO 27001:2013
This is why we are one of the most trusted solutions partners in the US healthcare ecosystem.
Customizable and Flexible Healthcare Payer Technology Solutions

Solutions for administrative workflows
- Claims management, auto adjudication
- Benefit administration and premium billing
- Robust member and eligibility management
- Workflow automation with real-time bundling/ unbundling
- Provider administration/ referrals & authorizations

Apps for enhanced business outcome
- Self-service applications for customers
- Provider portals with automated adjudication
- Automated claims processing application with high volume EDI support
- Custom applications according to requirement

Payer solutions for provider networks
- Use our nationwide connectivity to streamline engagement and claims processing
- Enable pharmacy benefits administration to optimize member experiences and financial outcomes
- Convert to e-payments to lower reimbursement-distribution costs
- Achieve accurate, risk-adjusted payments to meet compliance and quality goals
Benefits of Our Solutions
Our healthcare payer solutions offer a wide range of benefits designed to optimize your operations and enhance member experiences. By choosing our services, you can expect:
Streamlined Operations
Our solutions are designed to streamline your administrative processes, reducing manual work and improving efficiency.
Enhanced Member Experience
With our solutions, you can provide your members with seamless experience, from enrollment to claims processing, leading to higher satisfaction rates.
Improved Cost Management
Our solutions help you manage costs more effectively, reducing overheads and ensuring optimal resource allocation.
Advanced Analytics
Gain valuable insights into your operations and member behaviors with our advanced analytics capabilities, allowing you to make informed decisions.
Compliance and Security
Ensure compliance with regulatory requirements and protect sensitive data with our secure solutions.
Scalability
Our solutions are scalable to meet your growing needs, ensuring that you can easily expand your operations without compromising on performance.
Other Areas we Excel in
We help achieve your business goals via the optimal use of technology and expertise.
Integrate with FHIR Standards
Enhance EDI Capabilities
Automate Business Process/Testing
Empower Business with Technology
Operational Efficiency with Cognitive Services
Nalashaa has worked closely with the US healthcare industry for over a decade.
Our solutions have enabled over a billion error-free transactions for healthcare payer organizations. Here is what you can expect from us every time.
Healthcare Ecosystem Experience
Decade logn Experience in US healthcare
Complete Trasnaparency
Enabled by a culture of accountability and ownership
Tangible Quality
Showcased through metric-driven processes
Competent Healthcare IT Partner
Tactful health Management solutions
Global Delivery Model
Maximum value with risk diversification
Let's spark innovation!
Experience Payer Ecosystem
How We Stay Ahead of Competition
Healthcare Ecosystem Experience
We focus on US healthcare
Complete Transparency
Enabled by a culture of accountability and ownership
Tangible Quality
Showcased through metric-driven processes
Competent Healthcare IT Partner
Tactful health management solutions
Global Delivery
Model
Maximum value with risk diversification
Let's spark innovation!
Let's spark
innovation!
Be it technology or regulation in the healthcare payer ecosystem, connect with us for expert opinions.
Improve your claim and care management through an expert technology partner.
Worth Exploring
A glimpse of our industry expertise
Frequently asked questions
1. What are payers in healthcare?
Payers in healthcare refer to organizations or individuals who pay for healthcare services on behalf of patients. These can include insurance companies, government agencies such as Medicare and Medicaid, employers, and individuals who pay out of pocket for healthcare services. Payers are responsible for reimbursing healthcare providers for the cost of services rendered, and they negotiate rates with providers to ensure that costs are reasonable and affordable. Understanding the role of payers in healthcare is important for both patients and providers, as it can impact the cost and accessibility of healthcare services.
2. Is it payer or payor?
Both "payer" and "payor" are used in the healthcare industry to refer to entities that pay for healthcare services. However, "payer" is the more commonly used spelling in the United States, while "payor" is more commonly used in British English. Despite the difference in spelling, both terms have the same meaning and refer to the same concept. Understanding the difference between payer and payor is important for healthcare professionals and patients who need to navigate the complex healthcare system and insurance industry. It is crucial to use the correct spelling in your communications to ensure clarity and accuracy.
3. Who is the largest payer in the US healthcare industry?
The largest payer in the US healthcare industry is the federal government, primarily through the Medicare and Medicaid programs. These programs provide health insurance coverage to millions of Americans, including seniors, low-income individuals, and people with disabilities. Private health insurance companies also play a significant role in healthcare payments, particularly through employer-sponsored plans. However, the government's share of healthcare spending is expected to continue growing in the coming years, as the population ages and healthcare costs continue to rise.
4. What are the examples of healthcare payer software?
There are various examples of healthcare payer software, including Payer Care Management Solutions, CMS Payer Interoperability Solutions, Claims and Administration Platforms for Payers, CRM for Payers, Payer Quality Analytics Solutions, and Risk Adjustment Solutions for Payers.
5. What are major healthcare payer companies?
Some major healthcare payer companies in the United States, including government entities, are Centers for Medicare & Medicaid Services, UnitedHealth Group, Anthem, Aetna (a CVS Health company), and Blue Cross Blue Shield Association.
