Our client, a leading chiropractic EHR and Practice Management Software provider, approached Nalashaa to modernize the billing processes. Serving 7000+ healthcare practices, they needed a streamlined system for routing claims to appropriate clearinghouses based on insurance plans.
Too many Pathways Too many Problems
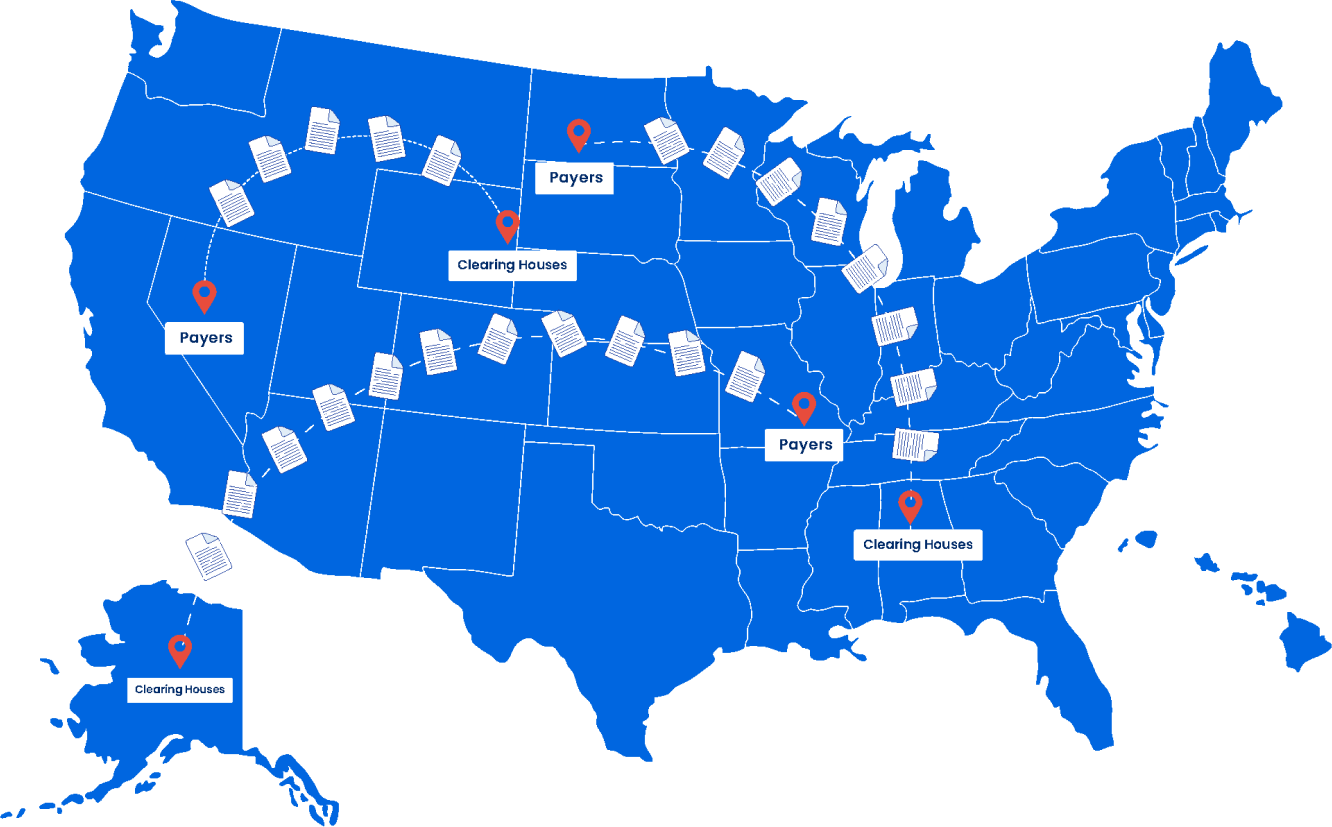
Clearinghouses play a pivotal role in exchanging clinical / treatment related details electronically to payers across a secure channel, armoring the healthcare ecosystem with the essentials to process claims efficiently. They increase efficiency by reviewing benefit details, validating coding accuracy, processing and relaying claims among payers. Our client wanted us to migrate the capability from a client-server model to a cloud platform improving efficiency & accuracy of submissions.
It was an immense undertaking, navigating through a torrent of transactions, expansive payment networks, diverse patient plans based on provider, place of service (location), and services rendered. Added to this complexity were the stringent security protocols dictating the exchange of PHI data to precise payer systems, leaving no margin for error.
Sorting out the Pathways
Clearinghouses play a pivotal role in exchanging clinical / treatment Despite the complexity, the PMS system was integrated with the payer ecosystem through an intuitive plug-and-play interface. The interface empowered the provider and the payer manage the patient payment lifecycle by effectively routing claims to the right payer ecosystem This also mitigated the delays for each of these stages: eligibility verification, prior authorization, claims approval and claims remittance.
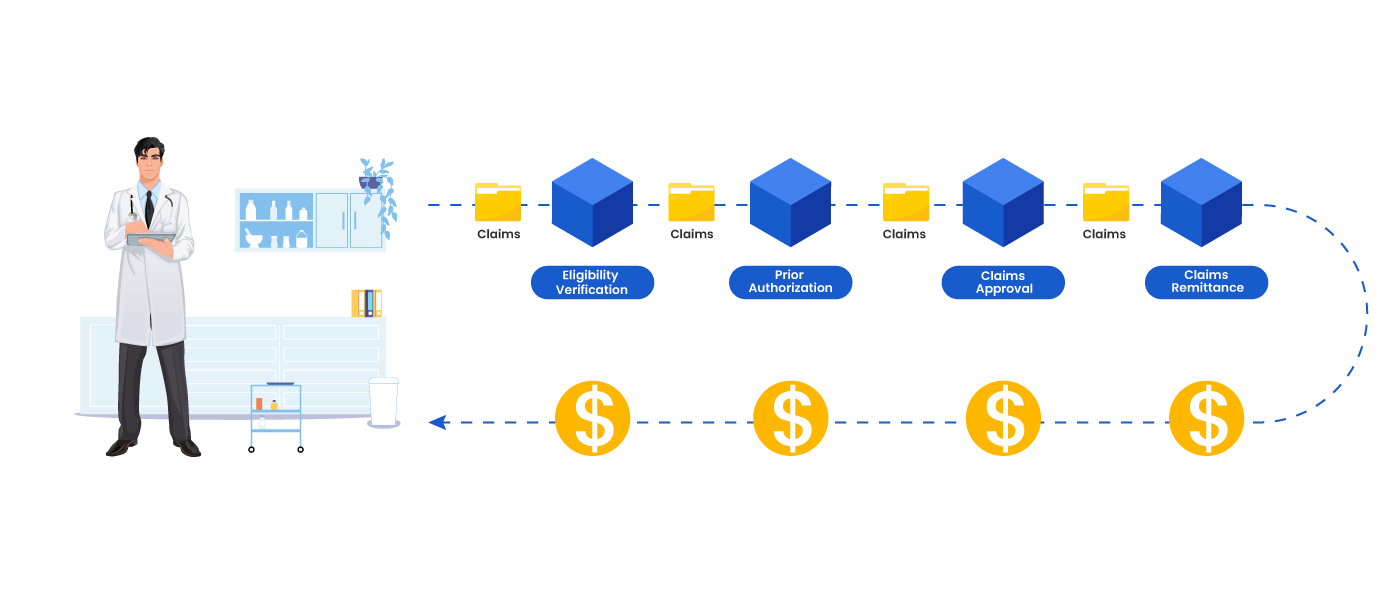
The system was also able to identify records that needed adjudication and initiate the automated claims processing workflow. Guided by treating doctor, payer and place of service details, the system intelligently identified the appropriate clearinghouse.
Top Highlights
Automated the tedious task of matching diverse health insurance coverages with the right payer systems through a plug-and-play dynamic interface
Offered the convenience of both SFTP and API calls for delivering files to the designated clearinghouses.
Achieved 95% automation in claims management
Set the stage for error-free reimbursements.
Technology Stack


Worth Exploring
A glimpse of our industry expertise