Plagued with Population Health Management Inefficiencies?
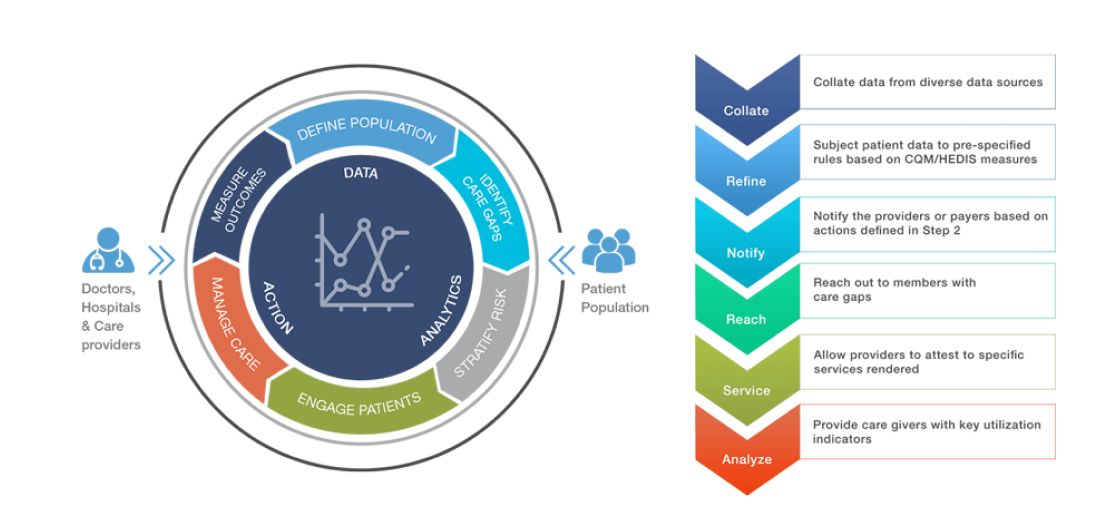
PHM is a systematic way of gathering, analysing and managing at-risk patients’ data through tools such as Utilization Management, Case Management, Disease Management, Portals etc.
Existing PHM solutions aim to achieve population health management goals for providers by identifying care gaps, preventing medical errors and improving patient outcomes. While it’s a vast improvement, there still exist challenges that need to be addressed
- Complex, inconsistent and inefficient workflows
- Manual and delayed Authorization Reviews
- Increasing employee fatigue from evolving policies/criteria
- Convoluted, time-taking and ever changing configurations
- Diminishing end user satisfaction (Patients/Providers/Payers)
Where you are headed, depends on where you are
Migration to value-based-care is forcing organizations across the US to become more competitive. In order to stay afloat they need to figure out ways to manage their financial risk. Depending on their risk appetite, most organizations are in one of the following phases when it comes to PHM adoption.
-
Clueless
about itIn order to arrive at what you need, you need to analyse what you want to do with it. With quite a few solutions out there, choosing the right one is crucial. We can help you look at things clearly.
-
Chosen a solution,
don’t know how to use itAligning solution workflows with your needs and way of working is vital to harness the true potential of PHM solutions. Configuring most PHM solutions is more than trivial.
-
Using it
& strugglingData inconsistencies, employee fatigue and workflow inefficiencies are the most common issues end users experience after adopting a PHM solution. We can reassess it and help you streamline things.
-
Successfully
leveraging itWell, congratulations for doing it all right! Maybe it’s time to figure out new frontiers.