A prestigious Urology Healthcare Facility in the US was on a mission - to revolutionize their Designated Fee Allocation (DFA) process. The DFA process, responsible for managing advance payments made by patients for upcoming appointments, was ripe for transformation.
Nalashaa, a seasoned technology partner, was chosen for this task. Their mandate was clear - to design an automated system to manage patient advance payments with precision and efficiency.
The Challenge
For the facility's front-desk personnel or billing team, allocating these advance payments to the right visit was essential. This allocation ensured the correct reflection of a patient's payment on the claim generated for a specific visit. However, the DFA was a maze of complex steps - it was time-consuming and riddled with intricacies.
Having experienced Nalashaa’ s prowess in automating multiple processes such as Eligibility Verification, Anesthesia Claims Management, and Credit Balance Resolution, the facility decided to extend automation's benefits to DFA.

The Solution
Nalashaa introduced a bot that redefined efficiency. Each day, the bot sifts through new appointments, identifying those with an associated advance payment. It checks the designated amount and allocates funds accurately based on the service date and visit type. It's smart enough to handle duplicate appointments and bypass records that need no processing.
But the bot's capabilities don't end there. It updates the status of each record and sends a comprehensive job summary via email, ensuring seamless communication and documentation. What's more, it completes this entire process within a remarkable 10-15 minutes.
The Impact
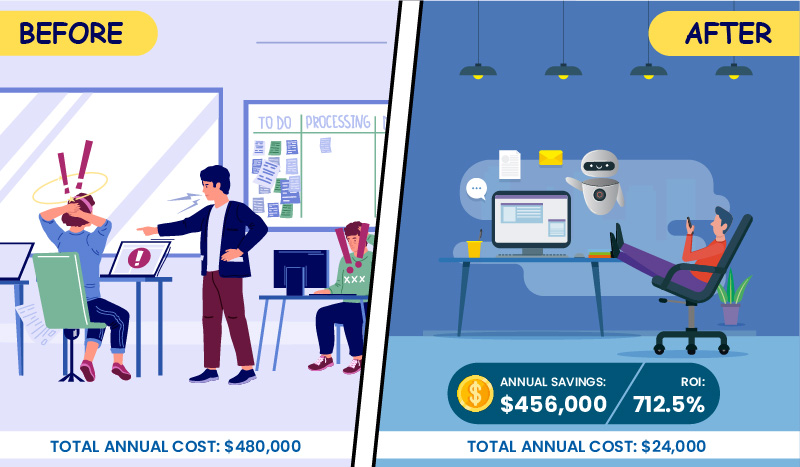
The implementation of the bot ushered in unprecedented efficiency in the DFA process.

Tasks that previously took a taxing hour were now accomplished in under 10 minutes.

The bot not only enhanced the billing team's productivity but also significantly improved the allocation process's accuracy.
Technology Stack